"I will never get over seeing whole families and healthcare workers die": Bearing witness to the experiences of NHS staff during the first pandemic year
The reality of the first year and its aftermath: (anonymous) testimony from staff at the NHS front line
“Staff sitting in literal cupboards crying alone because staff weren’t allowed to sit together & we couldn’t take all the death around us. It was utterly traumatising”
The pandemic is not gone but it is largely forgotten. Especially the first year, with its two devastating waves in which over 140,000 people died. The NHS reorganised itself completely to deliver care to the thousands of very sick Covid patients, alongside continuing care for other patients throughout. The system strained and buckled and staff were pushed to their limits and beyond. The impact continues today as the NHS is weaker, less resilient and with much longer waits than before.
In the summer of 2020, after the first wave, there were already high levels of PTSD, anxiety and depression in ICU staff. A 2022 survey by NHS Charities Together estimated that 60,000 NHS staff might be living with PTSD because of Covid. Nine out of ten respondents said it would take them years to recover from it.
The official NHS line in the autumn of 2020 was that the NHS coped and did not run out of intensive care capacity. In the Inquiry last month, Lord Stevens (head of the NHS for most of the pandemic), also implied that the NHS was not overwhelmed - to the anger of many who had served on the frontline.
In this post, I want to bring you back to the reality of the Covid pandemic for NHS staff in that first year. Firstly, with a brief overview of the data. Secondly, through testimonies of NHS staff in their own words from an anonymous survey that I started this week. The survey remains open for anyone who wishes to participate.
The pain and anger is palpable and raw in almost all responses. Many talk of the devastation of moral injury - the injury of working in an environment where your values are violated - for instance knowing you cannot provide all the care that patients need.
I highlight a range of testimonies in this post, but they all available in full in this PDF document: NHS frontline experiences.
The context of that first year
When the first wave of Covid hit us in March 2020, there was no treatment and no vaccine. It was both more infectious and more deadly than flu. There was a shortage of Protective Personal Equipment (PPE) in England, even as staff were redeployed to the NHS front line and intensive care capacity was rapidly and massively expanded. Excess mortality in the first wave among working-age adults was highest in healthcare workers.
Eight months later, the NHS - and its staff - not only had to do it all over again, but it was even worse, with more admissions to hospital, more use of critical care, and more deaths. The vast majority of people had not been vaccinated, the Alpha variant which emerged in December 2020 was more deadly than the original strain, and treatments remained limited even though options had improved since the first wave. Vaccines for healthcare workers only started in January 2021, just as the 2nd wave was peaking.
Huge increases in intensive care use for Covid patients - who were incredibly sick
Both waves saw the overall number of people receiving intensive care in England (for all diagnoses) far exceed non pandemic levels - 33% higher in the first wave and 66% higher in the second wave.
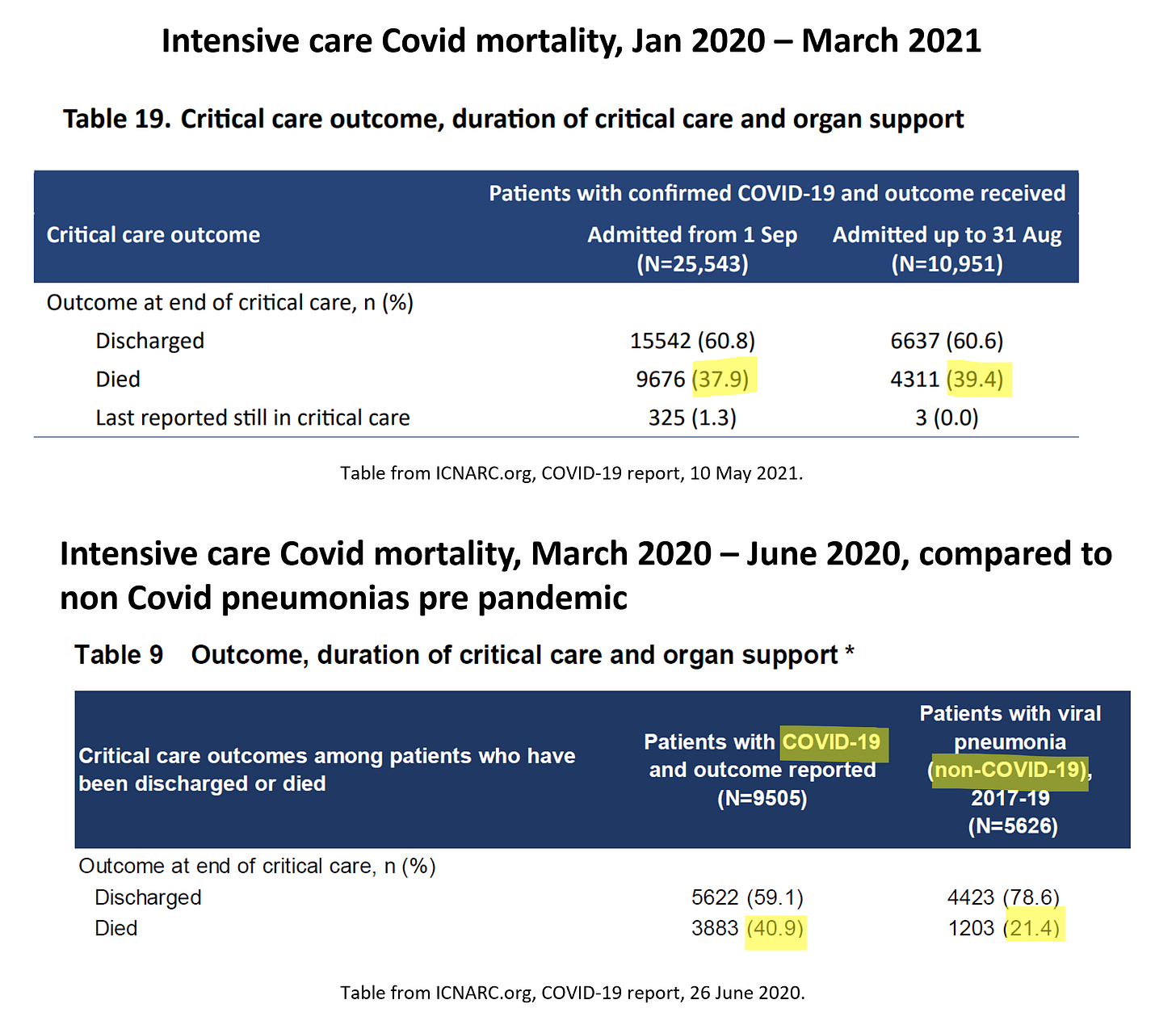
And Covid ICU patients were so sick. The mortality rate from Covid-19 was far higher than for ICU patients with other pneumonias, pre pandemic. Almost 4 in 10 Covid patients admitted to ICU in the first two waves died, compared to 2 in 10 for non-Covid pneumonia ICU patients.
We also know that mortality was highest in patients treated in surge intensive care areas (i.e. in areas rapidly redeployed to deliver intensive care), and highest during the wave peaks.
Impact on NHS staff
I have already pointed to a 2022 survey on the ongoing trauma, anxiety and depression experienced by many NHS staff. The recent Inquiry hearings on the first year left many NHS staff upset at how little acknowledgement there was of what happened on the frontline - all while we heard about the chaos in leadership, that covid rules were rarely followed in Downing Street and excuses for parties.
Before Module 3 of the Inquiry starts, which deals specifically with the NHS, I wanted to do what I could to bear witness to what it felt like at the time - and what it still feels like now.
Below are just a few excerpts from the testimonies of 111 respondents who were on the NHS frontline during the first two waves from my anonymous survey. Especially in the first wave, the strain was not felt equally across the country, and experience varied across the respondents. I also do not claim respondents are representative of all NHS staff, but I suspect they speak for a great many. Their pain, fear, anger and sadness deserve to be heard.
All 111 responses (to date) are available in full in this PDF document: NHS frontline experiences. The survey remains open for anyone who wishes to participate and I will update the linked PDF accordingly.
Please read and share.
What was it like?
Consultant palliative care doctor: “It broke my soul. The distress and pain of policing rules when trying to look after dying people and having limits to visiting. It was too much, too painful.”
Consultant surgeon: “I worked as an the Intensive Care Unit nurse in the Jan 2021 surge for 5 weeks. That was more traumatic than having COVID.
My ICU colleagues were burnt out, clinically depressed, and crying at work. I do not know how they did this for two years.”
Ambulance staff: “Terrifying - I didn't know if I could be protected adequately at work, I was scared of bringing the virus home to loved ones. I was subjected to abuse from covid deniers, I had to continue to work in an understaffed environment with poor ppe. Family and colleagues died and I couldn't attend funerals or grieve.”
Surgeon seconded to intensive care: “Saw a man one day on [intensive care] who’d lost his mum and his brother due to covid and his sister was an inpatient - I tried to get him to FaceTime his sister - he didn’t want her to see him struggling , persuaded him to write a note to pass to her - he was intubated the next day and died . I’ll never forget him . At times one of us looking after four patients on ITU so others could [go] drink water and go to toilet .We cried , we came home exhausted . We were overwhelmed”
Clinical nurse lead: “It was like a war zone Very stressful Cleaners wearing makeshift ppe Patients left alone on wards because of infection risk”
GP lead for over 1000 care home patients: “Harrowing, exhausting and unsupported. The first few weeks of what we saw in care homes was unseen (even denied) by the public and policy makers despite trying to highlight what we knew would happen weeks in advance”
NHS Speech and Language Therapist who volunteered to help on intensive care: “I’d never been in an the Intensive Care Unit…I’d never watched someone die. I sat with patients and held their hands as they died. I sat with families as they came and said goodbye. I spoke to them, washed them, talked to them. Then with the nurses put them in body bags. I supported them to say goodbye on FaceTime. I learn to change ventilator settings, to get oxygen masks on them. It’s was scary beyond belief.”
Consultant doctor: “The second wave was horrific - patients were so sick and we had nothing to help them (I work in geriatrics)… and we just had to watch people die. The consultants (where I worked) kept the trainees out of the bays (we communicated via walkie-talkie) so it was only us really who saw the patients. My ward had 50% mortality and there was nothing I could do. I will never get over it.”
GP: “Scary, constantly changing, felt out of control and no one listening, no PPE, exhausting, worrying, patients we knew dying or terrified, lack of sense that anyone knew what they were doing.”
NHS IT project manager: “I cried twice a day every day for a month. Once on the way into work and again on the way home.
Life was wake-up, go to work, deal with hell - not knowing if you were going to catch it yourself, go home, sleep and repeat.”
Paramedic: “Scary. Seeing how quick patients were deteriorating in front of me was awful. Families knowing there was a big chance they would not see their loved ones again as I took them to hospital in the ambulance. I often worked as a solo responder and on several occasions I was waiting for backup with very unwell patients and running out of oxygen and having to ration it to try and make it last till my backup arrived.
The worst was when patients were too scared to call. I had patients beg me not to take them to hospital as they feared dying of Covid in there.”
Hospital physiotherapist: “Horrific and terrifying. If I didn't have my colleagues and assistance to get counselling I would not have gotten through.”
Community nurse: “It was very, very frightening. I had never seen something this lethal and nothing we could use against it. Getting hold of anything (PPE) to protect yourself was difficult and rationed for other NHS staff. After 33 years in nursing, I couldn’t believe the lack of reaction from the government to protect us”
Senior Neonatal Intensive Care Nurse: “Horrendous. I barely slept, when I woke up in the morning I obsessively checked how many new cases and new deaths there had been, whether it was going up or down. I often cried myself to sleep. At 27, I had to question whether I - like many other health care staff - would die.”
What is the ongoing impact on you or the NHS?
Lead Radiographer: “I don't think any of us are the same. Particularly now we know how those imposing the rules on us ignored them and carried on as usual.”
Nurse: “Personally PTSD. I still have flashbacks but generally morale is crushed. My Colleagues have had enough. Anger. Sorrow for the patients that we couldn't have done better for them.”
Senior nurse: “Staff have PTSD. Regular talk of before and after covid. It’s like a massive blot in time.”
Radiographer: “My team were just exhausted from all the extra shifts but were put under huge pressure from those who hadn’t had such a hands on role when the recovery period started. We asked for help and support but we’re accused of delaying recovery and cancer targets unless we continued to work all the extra shifts.”
Senior Neonatal Intensive Care Nurse:“I developed severe anxiety and needed counselling. Nurse and doctor friends have since struggled with issues of PTSD, had time off work because of their mental health, left the profession altogether and even attempted suicide (some of which were successful). My best friend - a senior intensive care nurse, was diagnosed with PTSD and spent weeks in bed, unable to sleep for nightmares of what she described as a conveyor belt of people dying, gasping for breath…
I cried when I had my first vaccine. I felt such a sense of relief. And yet I still had to face the anti-vaxxers and the deniers who called me a liar. Then with the nurses strikes I watched the prime minister describe us as money-grabbing and selfish, while I remembered the staff who are either permanantly disabled with long covid, mentally traumatised, or dead. After everything we had all been through, it rubbed salt in the wounds.”
Palliative Care: “Now people seem to have completely forgotten the nightmare we went through”
GP: “The impact of covid was a driver for my early retirement”
Community nurse: “I eventually got [Covid] in July 2022 and was very ill. My husband is clinically vulnerable.... As an older person I have been infuriated with a government who sees me as expendable collateral: their brutal, crude handling of the pandemic and the way they treat us employed in the NHS with contempt and disdain has made me view them with hatred.”
Paramedic: “Drained and burnt out. Leaving frontline healthcare for a support role in the same trust. Going forward I don't want to face another horrid winter in the NHS”
Staff nurse: “Developed Long Covid. HR wanted me to take Ill health retirement. HR kept discussing fitness to continue in role without giving chance for recovery.”
Surgeon seconded to intensive care: “I will never forget or forgive how the pandemic was managed in the early stages. This caused many deaths. People close to me have said "get over it" I will never get over seeing whole families and healthcare workers die.”
GP: “My capacity to handle stress has vanished significantly now. My mental health has been impacted. I have not stopped working though, went part-time for a while, which helped.”
Nurse: “The NHS was struggling to meet the needs of our patients before the pandemic but now it is so much worse. Waiting lists are so long I fear we will never be back to pre pandemic levels”
Neurosurgeon: “I was a surgeon in a high prevalence area. We filled our pension death benefit forms in as a group.
I caught Covid at work early on and thought I might die. At this point, policy was not even to contact 111 unless requiring an ambulance. I wrote a will. My residual symptoms lasted for months.”






This made me cry. I worked in NHS mental health services at the start of the pandemic but I left, as there was an expectation to just carry on with no protection as we were not on the Covid frontline. As someone with co-morbidities I was not prepared to risk my health in that way.
This article brought it back to me how frightening that time was, and how we can’t just move on from this and pretend that life has gone back to normal. Covid has left massive scars and psychological trauma that will cast a long shadow. This alongside the very real physical issues that are ongoing from Covid.
Truly tragic.
Certainly history is being rewritten, particularly in the right wing press. I wasn't in a front line area of the NHS but the impact was still enormous. Nobody knew what the virus was going to do, how many would die, or what Government policy was. The debate around the Excel centre was initially would it be a factory scale morgue. Training of doctors nurses dentists etc was suspended as they were shifted to direct patient care. Everybody was working ridiculous hours to try and reorganise. I used to think Simon Stevens was a good advocate for the NHS compared to his predecessors but after his appearance at the Select Committee I wonder if he had a clue.
And now we are back to the Treasury wanting "financial balance" as its priority. I'm glad I retired.