Only luck will prevent a repeat of last winter's collapse in NHS emergency care
Can we avoid a repeat of last year this winter? Probably, but not because we've done anything to prevent it.
The latest performance indicators for the NHS in England are out and they don’t make comforting reading. Indicators across all domains - ambulances, A&E, treatment & diagnostics - have been consistently and markedly worse since the pandemic and winter is when the NHS is always most stretched. However, there is a terrible winter (winter 2021/22) and then there is a catastrophic one (winter 2022/23). It’s estimated 500 more people died every week in December 2022 directly because of delays in emergency care. And the bad news is that so far autumn 2023 looks more like 2022 than 2021 for some key metrics.
Despite some additional government cash for this winter, the NHS is not in better shape this year than last. This means that the biggest factor in avoiding last year’s catastrophe will be avoiding a triple spike of Flu, Covid and RSV infection. And that is down to luck - not a particularly comfortable place to be.
Read on for a dive into some of the NHS indicators and a look at current Covid, Flu and RSV trajectories. Thank you as ever to Bob Hawkins for his help with many of the slides.
Ambulance care
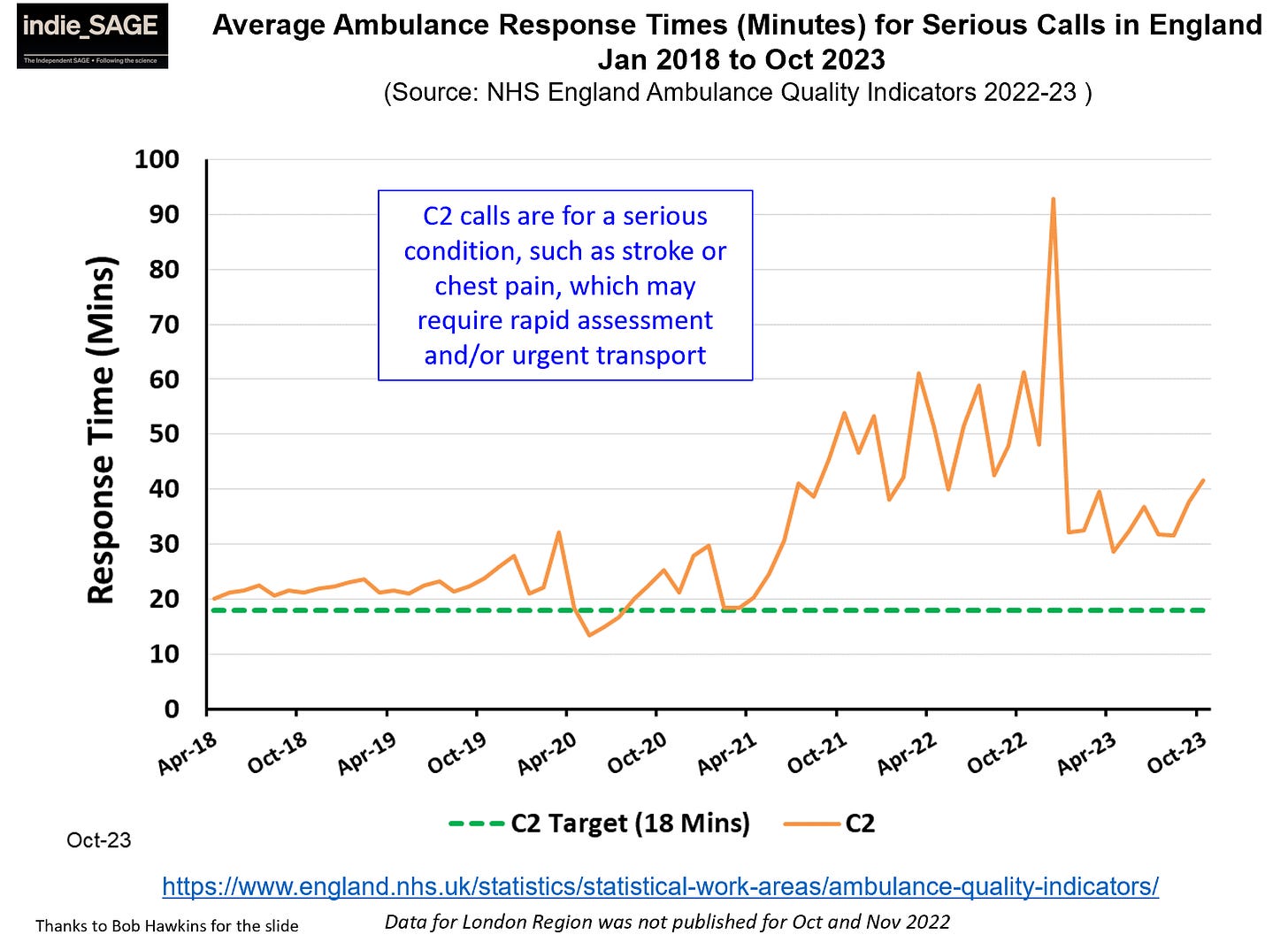
Ambulance response times to call outs went up last month. For instance, response times to category “C2” calls for serious problems like suspected stroke or heart attack are running at about 40 minutes - more than double the target of 18 minutes.
A key metric of stress is ambulance handover time which is only reported during winter - this will be available in a few weeks, but we are already seeing stories of long delays at some hospitals.
A&E waits
A&E waits increased sharply in October, whatever measure you choose. Last month, 30% of patients waited longer than 4 hours from A&E arrival before either being admitted or discharged. Compared to the last few winters, this year is far closer to last year’s highs than it is to any other year.
Over 8% of people waited longer than 12 hours for admission after a decision to admit them, only just below 2022’s 9% and far higher than 2021’s 2%.



Hospital treatment
There are almost 8 million referrals waiting for treatment in the NHS at the moment - a record number. For the first time, the NHS has now also given the number of individual people waiting for treatment - a massive 6.5 million people (many are being referred for more than one thing, so this number is smaller than the total number of referrals).
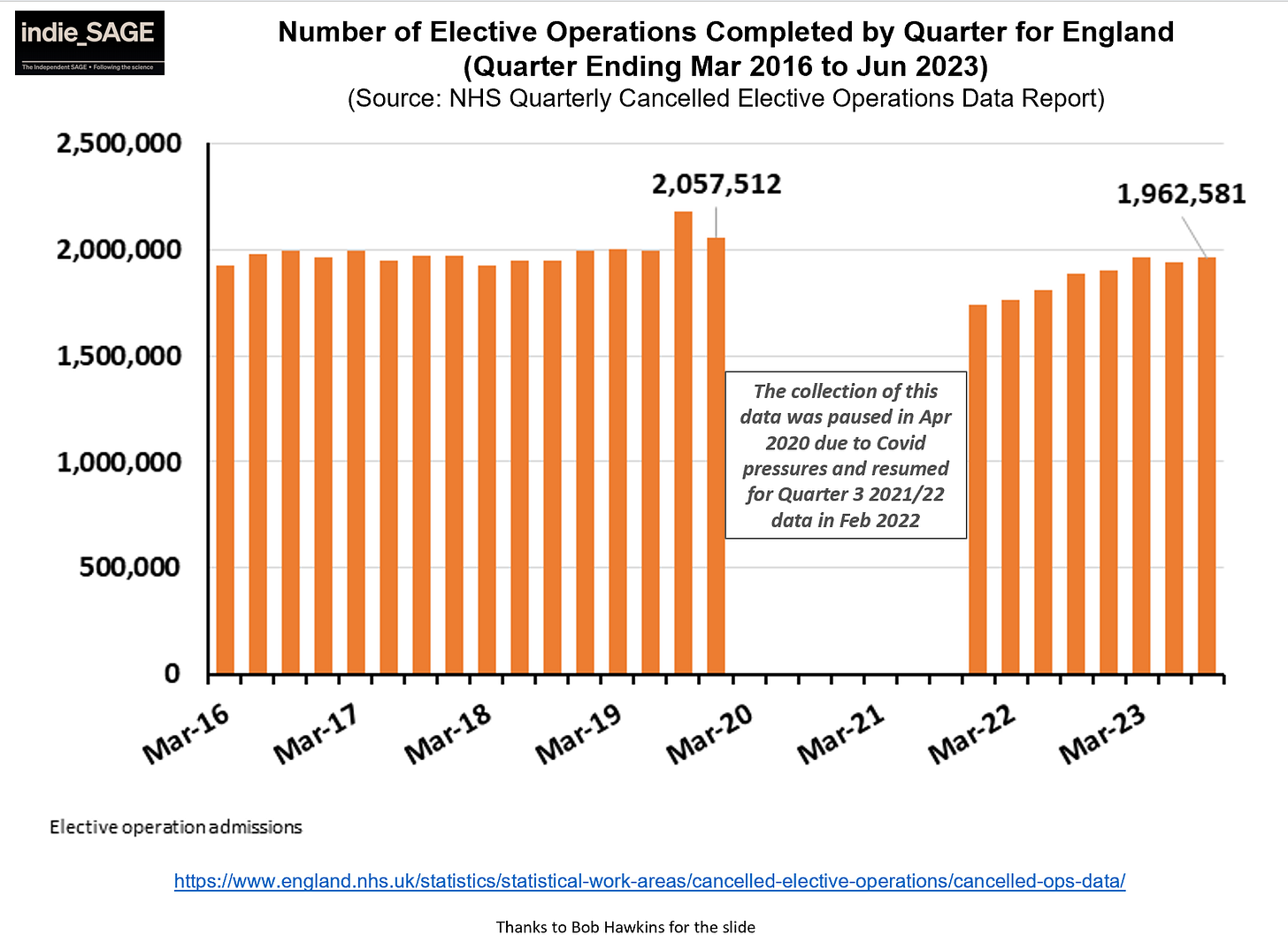
Unfortunately, while NHS activity has ramped up since the pandemic, it is still not at pre-pandemic levels - and without significantly exceeding pre-pandemic activity, it’s hard to see how the waiting list will come down.
Diagnosis
Diagnostic waits remain high and for key indicators such as cancer, they are moving in the wrong direction. A quarter of patients are waiting longer than 2 weeks to see a consultant after an urgent GP referral and 40% are waiting longer than 2 months to start treatment - both metrics far above their target.
These longer waits will be causing a lot of anxiety for many patients and will lead to worse clinical outcomes for some.


Staff context
NHS staff are exhausted, demoralised, and angry after the brutal pandemic years. This year a cost of living crisis and a decade of stagnant wages in the face of inflation added severe financial pressures. The NHS is about to enter winter after a year of unprecendeted strikes from ambulance staff, to nurses, to junior doctors to consultants.
In my recent survey, many spoke of their fear for the NHS and their own capacity to cope. Some had already left. NHS staff simply do not have the emotional or physical capacity to go above and beyond in the way they have done previously.
Intensive Care Nurse: I left the NHS and moved abroad - it had been on the cards for a while but the way the government treated us in the pandemic sealed my decision. I still have flash backs to Easter 2020 in particular and find it traumatic to talk about. … I find it incredibly sad talking to colleagues who are too burnt out to continue or care anymore. This government broke not just the NHS - it broke us.
Nurse: The NHS was struggling to meet the needs of our patients before the pandemic but now it is so much worse. Waiting lists are so long I fear we will never be back to pre pandemic levels
Paramedic: [I’m] Drained and burnt out. Leaving frontline healthcare for a support role in the same [ambulance service]. Going forward I don't want to face another horrid winter in the NHS.
Consultant doctor: I still cry. I have panic attacks when I think about [the first year of the pandemic]. My morale is low. But as a senior member of staff, I have to stay strong and keep going . I am not sure whether it is a comfort or terrible thing that so many staff I talk to feel the same way. So many staff are broken.
Will we get lucky?
Last December we had a triple peak of Covid, RSV and Flu, which overwhelmed NHS emergency care capacity.
We have a much better chance of avoiding last year’s crisis if we can avoid this - either by the three respiratory illnesses peaking at different times or by at least one peaking at much lower levels. So how is it looking?
The bad news is that RSV admissions are as bad, or worse, than last year. But the good news is that Covid admissions are lower (even allowing for less hospital testing) and Flu admissions are much lower.



While it is still quite possible that one or both of Covid and Flu will have signficant December surges, it is looking much less likely that both will. Therefore, if I had to guess, I would say the NHS will scrape through this winter better than last year - but not because of more money, more staff, or better systems, but only because of a chance pattern of infectious disease.
Going forwards, we must push for more support for the NHS in the short and long term, take back control of its fate in winter, provide relief to its exhausted workforce and better, more timely, health care for those in desperate need.






When I was younger I never thought about what might happen if I needed urgent medical care. It was just there. Now, as I get older and look down the barrel of ageing with a chronic illness I have tried to fix for 10 years unsuccessfully, it scares me to know that my parents had the best of the NHS. They never doubted it for a moment. That time has gone. I'm worried.
Thanks for this distillation of NHS England's data.
One glaring weakness in their data though is the willful ignoring of community demand. Since 1990 UK has focused almost exclusively on the needs based aspects of service delivery, whilst ignoring that needs reveal themselves either from demand or from screening. Whilst screening activity is closely followed, demand is studiously ignored. Thus we have delays to contact GPa and queues to get into A&E. With Ambulance services reflecting the dusfunction of the demand response arm.
One thing is certain, if you ignore a problem it will eventually overwhelm everything else as CoVID demonstrated.
I know it's not in your gift to change what NHSE collects but perhaps we should all focus our attention on restoring the health of our primary care system for a while, not merely asking it to behave like an out patient department in the community.