Where are we with Covid in England & a plea for changing vaccination policy
Short term things are getting better, room for improvement longer term
Current Covid wave has peaked
The December/January Covid wave driven by new variant JN.1 (now about 90% of sequenced cases) seems to be over.
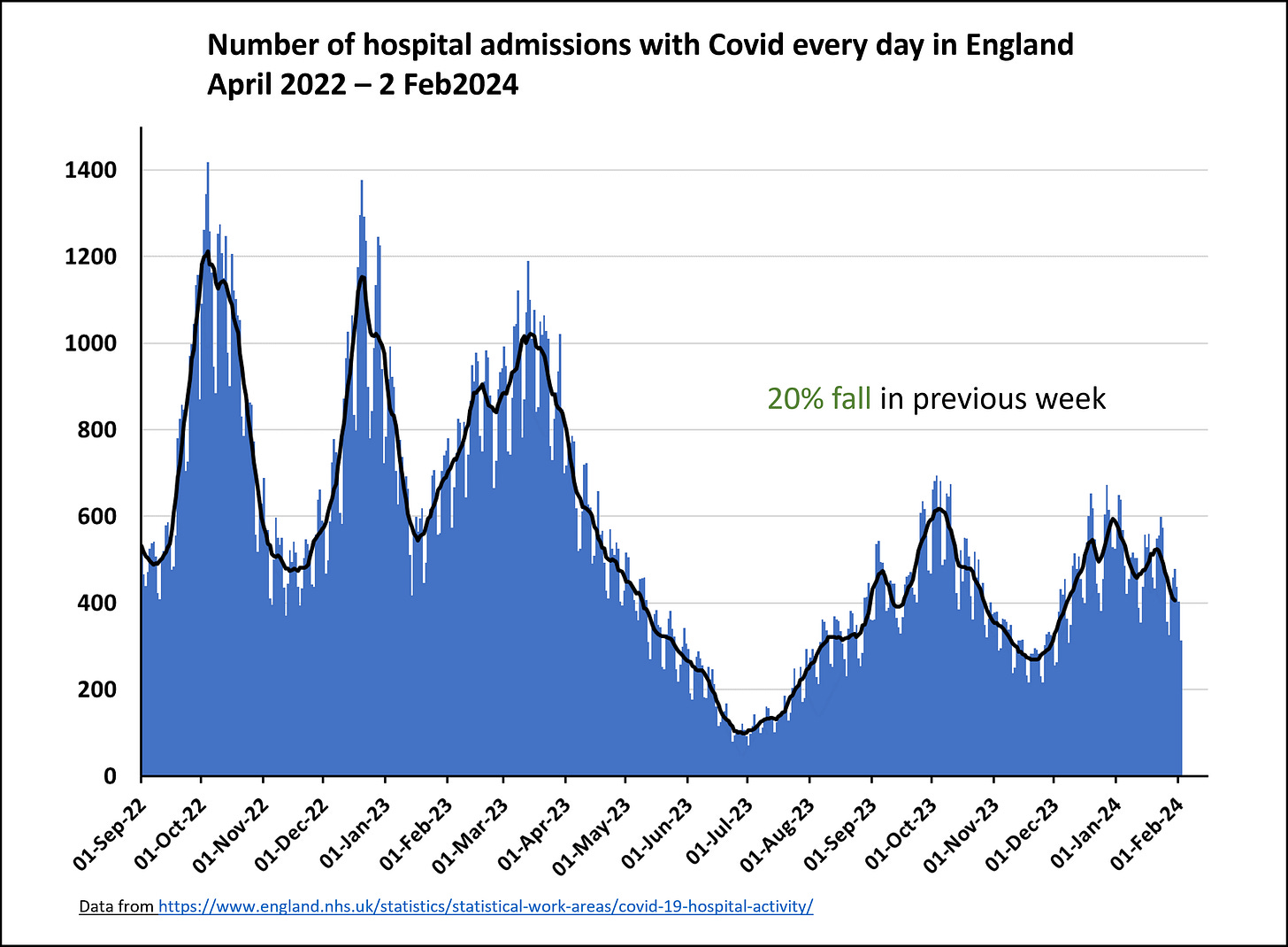
While the most recent ONS winter infection survey (which does not depend on test seeking behaviour) showed a small increases in cases, the latest data is now almost 3 weeks old (data up to 24 Jan 2024). More recent hospital admission data shows a definite downswing, with a 20% drop in the most recent week (up to 2nd Feb).
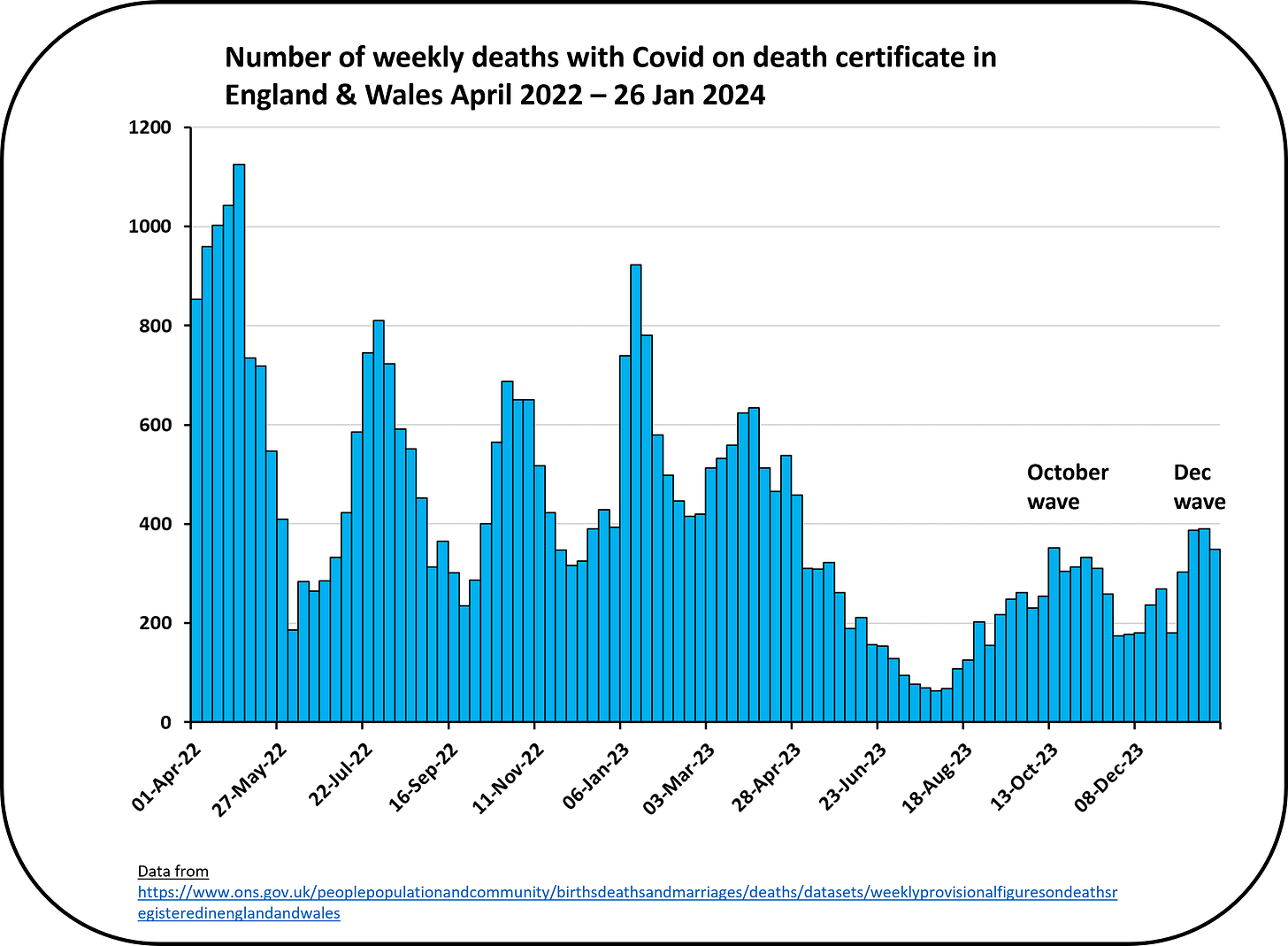
The most recent data on deaths with Covid on the death certificate (i.e. a contributing cause of death) is so far showing the first of the December peaks. Because deaths typically happen a few weeks after infection, it’s likely we’ll see another (small) increase from the second mid January peak before seeing a sustained fall. That said, Covid deaths from acute infection are far fewer now than even a year ago and that has to be good news.
NHS remains under pressure but last year’s awful crisis was not repeated
Overall, the NHS was lucky to avoid last year’s triple whammy of RSV, Flu and Covid all hitting in December - and in particular, lucky to avoid a repeat of the very very high December 2022 Flu wave. Instead, this year, while we had both a lot of Covid and Flu admissions in December/January, they were well below last year’s levels which reduced acute pressures.
That said, the NHS remains under pressure. Ambulance handover times (which are an indicator also of ambulance response times) remain high and are now higher than last year’s relatively quiet January - see Paul Mainwood’s analysis below, with more detail in his substack.
The latest NHS indicators more broadly should be published this week - follow Bob Hawkins’ substack for the detail on those - but we know for instance that cancer services remain under enormous pressure.
Looking ahead - Covid vaccination policy
JCVI (the UK vaccine recommendation body) just announced its recommendations for the Spring 2024 campaign, and it’s more restricted than last year. This continues the trend of JCVI gradually withdrawing the Covid vaccine offer from the population.
Most adults under 50 were last eligible for a booster two years ago. Fifty somethings last got boosted in the autumn of 2022. Children remain mostly unvaccinated (particularly under 12s) and they cannot be vaccinated (even for the first time) unless they have one of a relatively restricted set of health conditions.
The UK position thus seems to be to expect more and more people to get Covid pretty much every year, with little protection now from vaccination at all. And I, at least, find this concerning for the following reasons.
Long Covid
The JCVI risk-benefit modelling for the vaccine offer ignores Long Covid completely. This is despite plenty of evidence now that vaccination protects against Long Covid, as yet another large study published in January confirmed. They showed that vaccination reduced the chance of developing Long Covid by about 30%-50% and concluded that “Vaccination against COVID-19 consistently reduced the risk of long COVID symptoms, which highlights the importance of vaccination to prevent persistent COVID-19 symptoms, particularly in adults”.
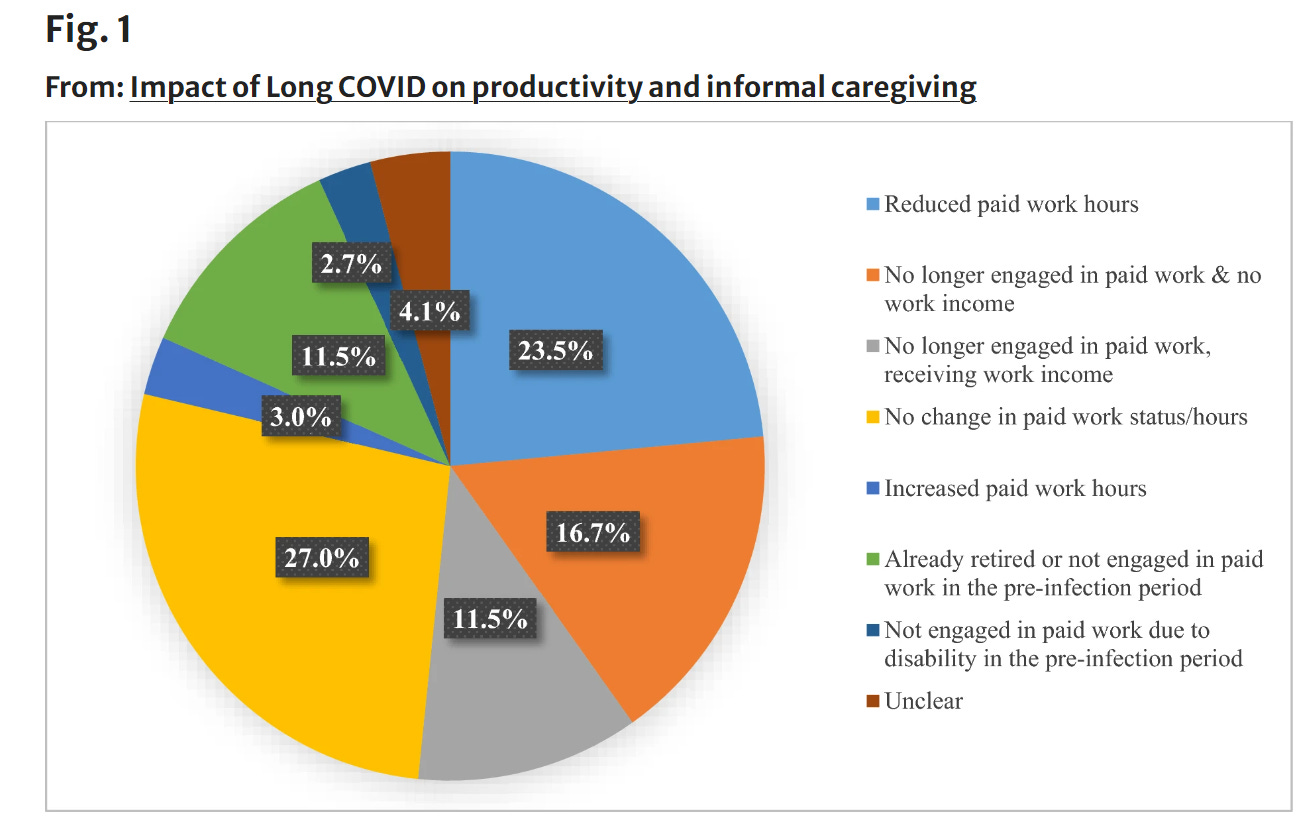
While rates of new Long Covid on infection are lower now that most people have had at least one previous infection, they are certainly not zero. We also know that the number of people out of the workforce due to chronic ill health is increasing and far higher than before the pandemic. While Long Covid is not the only contributor (NHS delays & increasing poverty also contributing), it certainly is playing a role. One recent survey highlighted the negative impact Long Covid has on people’s ability to work.
Not including Long Covid in the cost-benefit modelling is wrong.
JCVI cost-benefit models for deciding on vaccine rollout are not transparent
JCVI relies on bespoke modelling to underpin its recommendations for booster rollout, but the details of these models and the assumptions going into them are opaque. Just this week the Comptroller for the UKHSA accounts highlighted that this modelling must be far more transparent and that it is not at all clear that it supports JCVI advice.
One of the reasons given was that the main model was coded in the language Python and that they had to stop using it because the staff member that knew Python had left. The fact that decisions of this magnitude depend on one staff member knowing a particular coding language (which is very widely used by the way) is ridiculous and shows a frightening lack of resilience.
Vaccine wastage
We know that the UK ordered more vaccines than were needed in 2023 - and we are now facing the fact that we are about to throw away vaccines worth £229 million because they are out of date.
As the actuary John Roberts says “was [the fact we had so many vaccines] taken into consideration by JCVI when determining the cost/benefit analysis as to which age groups to offer vaccines to during 2023 and 2024 - if we were going to throw them away, why not expand the age groups eligible?”
Boosters and vaccines work! Including for children!
The boosters still work extremely well in reducing the serious acute consequences of Covid like hospitalisation and death, especially when updated against latest variants. This was true when BA4/5 emerged and remained true when XBB emerged last year. Vaccines also work extremely well in children - e.g. a recent study on adolescents in Scandinavia showed they reduced hospitalisations by 70%. The fact that no otherwise healthy children are now eligible to be vaccinated makes no sense, as I’ve written about before.
Vaccine policy is increasing inequality
From this Spring, two Covid vaccines (Novovax and Pfizer) will be available to buy privately for over 12’s - at about £45 per dose. I do think it’s good to have a private option if there is such a limited NHS offer, but the price point during a cost of living crisis means that many won’t be able to afford it. Given we already know that the risks of Covid are higher and vaccination rates lower for those in more deprived populations, this policy will inevitably make the risks of Covid infection more unequal across our population. This does not seem fair to me.
Summary
So, overall, the good news is that this Covid wave is on the wane and we avoided a repeat of last year’s terrible NHS crisis. However, I think we really need to rethink our strategy of just relying on everyone to catch Covid repeatedly as our only strategy. While reinfections may be less likely to lead to hospitalisations and deaths, they are still better avoided. Longer term issues such as digestive issues or heart problems remain important considerations.











Thank you so much for this. I really fail to understand the JCVI attitude to Long COVID... I have just read the terms of reference of the JCVI and I can see no reason for them to completely ignore Long COVID and it's health costs to individuals and economic costs to society. I wish they could be openly questioned on this.
Succinct and clear. Thank you. I wish BBC News website would ask you to write summaries like this. It would be so useful